Odisha State Board CHSE Odisha Class 12 Biology Important Questions Chapter 3 Human Reproduction Important Questions and Answers.
CHSE Odisha 12th Class Biology Important Questions Chapter 3 Human Reproduction
Human Reproduction Class 12 Important Questions CHSE Odisha
Very Short Answer Type Questions
Choose the correct option
Question 1.
Which organ’s outer covering is tunica albuginea?
(a) Testis
(b) Ovary
(c) Kidney
(d) Brain
Answer:
(a) Testis
Question 2.
Testicular descent to the inguinal region is effected by
(a) Testosterone
(b) LH
(c) AMH
(d) FSH
Answer:
(c) AMH
Question 3.
The temperature of scrotum is maintained by
(a) perspiration
(b) evaporation
(c) counter-current heat exchange
(d) All of the above
Answer:
(d) All of the above
Question 4.
Prostate gland in males lies
(a) inferior to bladder
(b) posterior to bladder
(c) anterior to bladder
(d) for away from bladder
Answer:
(a) inferior to bladder
Question 5.
Graafian follicle is observed in the ovary of
(a) rohu
(b) Amphioxus
(c) salamander
(d) human
Answer:
(d) human
Question 6.
If fertilisation does not occur. Graafian follicle is converted to which endocrine gland?
(a) Corpus luteum
(b) Corpus albicans
(c) Corpus spongiosum
(d) Corpora cavernosa
Answer:
(b) Corpus albicans
![]()
Question 7.
Glands of skene in females are
(a) greater vestibular
(b) paraurethral
(c) Bartholin
(d) homologous to male’s Cowper’s gland
Answer:
(b) paraurethral
Question 8.
Seminal plasma is rich is
(a) fructose
(b) calcium
(c) Both (a) and (b)
(d) None of the above
Answer:
(c) Both (a) and (b)
Question 9.
Corpus luteum secrete
(a) oestrogen
(b) progesterone
(c) relaxin
(d) All of the above
Answer:
(d) All of the above
Question 10.
Spermatids are
(a) motile
(b) immotile
(c) non-dividing
(d) dead
Answer:
(b) immotile
Question 11.
The part of sperm that gets embedded in seminiferous tubules after spermiogenesis is
(a) tail
(b) middle piece
(c) neck
(d) head
Answer:
(d) head
Question 12.
Egg mother cells are formed by
(a) meiosis
(b) mitosis
(c) Both (a) and (b)
(d) None of these
Answer:
(b) mitosis
Question 13.
Human egg is
(a) centrolecithal
(b) telolecithal
(c) alecithal
(d) macrolecithal
Answer:
(c) alecithal
![]()
Question 14.
From which part of spermatid is acrosome formed?
(a) Nucleus
(b) Mitochondria
(c) Golgi bodies
(d) Ribosome
Answer:
(c) Golgi bodies
Question 15.
Which type / types of cell division occur (s) in cells of testis at different phases of spermatogenesis?
(a) Only meiotic
(b) Only mitotic
(c) Both (a) and (b)
(d) Amitotic
Answer:
(c) Both (a) and (b)
Question 16.
During which stage of oogenesis the number of chromosomes is reduced to half?
(a) Formation of second polar body
(b) Meiosis-II
(c) Division of secondary oocyte
(d) Formation of first polar body
Answer:
(d) Formation of first polar body
Question 17.
On which day of normal menstrual cycle, ovulation occurs?
(a) 10 th
(b) 13 th
(c) 14 th
(d) 15 th
Answer:
(c) 14th
Question 18.
Generally, what is the site-of fertilisation in humans? (2022)
(a) Ovary
(b) Uterus
(c) Vagina
(d) Fallopian tube
Answer:
(d) Fallopian tube
Question 19.
During fertilisation through which path the male pronucleus moves to meet the female pronucleus?
(a) Penetration path
(b) Copulation path
(c) Migration path
(d)
Answer:
(b) Copulation path
Question 20.
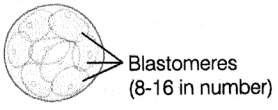
Name the cells formed by the division of zygote,
(a) Blastula
(b) Blastomeres
(c) Blastocoel
(d) None of these
Answer:
(b) Blastomeres
Question 21.
What is the correct sequence of embryo development?
(a) Gamete → Zygote → Morula → Blastula → Gastrula
(b) Gamete → Zygote → Blastula → Morula → Gastrula
(c) Gamete → Neurula → Gastrula
(d) Gamete → Neurula → Morula
Answer:
(a) Gamete → Zygote → Morula → Blastula → Gastrula
![]()
Question 22.
Human embryo is protected by which cavity?
(a) Am’niotic cavity
(b) Pleural cavity
(c) Peritoneal cavity
(d) Neural cavity
Answer:
(a) Amniotic cavity
Question 23.
What is the term used to represent the birth of a human foetus?
(a) Ovulation
(b) Abortion
(c) Conception
(d) Parturition
Answer:
(d) Parturition
Question 24.
Cleavage pattern is influenced by …………
(a) cytoplasm
(b) yolk
(c) nucleus
(d) centrosome
Answer:
(b) yolk
Question 25.
Embryo at 16-celled stage and without cavity is called …………..
(a) morula
(b) blastomere
(c) blastula
(d) gastrula
Answer:
(a) morula
Question 26.
What do you call the embryo at 16 celled stage?
(a) Blastocyst
(b) Morula
(c) Blastula
(d) Gastrula
Answer:
(a) Morual
Question 27.
LH surge is seen during
(a) menstrual phase
(b) follicular phase
(c) ovulatory phase
(d) luteal phase
Answer:
(c) ovulatory phase
Question 28.
Slow block to polyspermy is induced by
(a) vitelline membrane
(b) corona radiata
(c) zona pellucida
(d) All of the above
Answer:
(b) corona radiata
![]()
Question 29.
Pineal gland is derived from
(a) ectoderm
(b) mesoderm
(c) endoderm
(d) Both (a) and (c)
Answer:
(a) ectoderm
Correct the statements, if required, by changing the underlined words
Question 1.
Secretion of prostate contains fructose.
Answer:
Secretion of seminal vesicle contains fructose.
Question 2.
The primordial follicles are situated in the medulla of ovary.
Answer:
The primordial follicles are situated in the cortex of ovary.
Question 3.
Corpus albicans is an endocrine structure.
Answer:
Corpus luteum
Question 4.
Efferent ductules in males are 15 in number.
Answer:
12
Question 5.
Process by which sperms are released from seminiferous tubules is called spermiogenesis.
Answer:
Process by which sperms are released from seminiferous tubules is called spermiation.
Question 6.
Degenerated follicles are called Graafian follicles.
Answer:
Degenerated follicles are called atretic follicles.
Question 7.
Mitochondria in tail of sperms provide it motility.
Answer:
Microtubules
![]()
Question 8.
Corona radiata is the primary egg membrane. Fill in the blanks
Answer:
Zona pellucida
Question 9.
Three primary germ layers are formed during morula stage of embryonic development.
Answer:
gastrula
Question 10.
Intestine is derived from mesoderm.
Answer:
endoderm
Question 11.
The yellow coloured milk secreted by mother just after childbirth is called neonatal milk.
Answer:
colostrum
Question 12.
Fertilisation occurs in uterus.
Answer:
Fallopian tube
Question 13.
Gonads are derived from endoderm.
Answer:
Mesoderm
Fill in the blanks
Question 1.
Humans reproduce …………….. . (asexually/sexually)
Answer:
sexually
Question 2.
Humans are ………… (oviparous, viviparous, ovoviviparous)
Answer:
viviparous
Question 3.
Fertilisation is ………… in humans. (external/internal)
Answer:
internal
Question 4.
A thin ……….. separates the granulosa cells from theca interna.
Answer:
basement membrane
Question 5.
Rupture of Graafian follicle releases …….
Answer:
secondary oocyte
Question 6.
Each spermatogonium contains …………. chromosomes.
Answer:
46
![]()
Question 7.
Oogonia project into stroma of ovary as a chord called ………… .
Answer:
egg tube or Pfluger
Question 8.
FSH and LH are secreted by ……………. gland.
Answer:
pituitary
Question 9.
The sperm’s head gets embedded into ………. after spermiogenesis.
Answer:
Sertoli cells
Question 10.
Primary oocyte gets arrested at …………. stage of meiosis-I.
Answer:
diplotene
Question 11.
The fusion of male and female pronuclei is called …………. .
Answer:
fertilisation
Question 12.
During fertilisation, the sperm’s acrosome releases ……………..
Answer:
hyaluronidase
Question 13.
The covering of egg is called …………… membrane.
Answer:
vitelline
Question 14.
The primitive gut that forms during gastrulation is called ……………. .
Answer:
archenteron
Question 15.
The hormone …………. stimulates the secretion of milk.
Answer:
oxytocin
Question 16.
Zygote is ………….
Answer:
diploid
Question 17.
The process of release of ovum from a mature follicle is called ………….. .
Answer:
ovulation
Question 18.
Ovulation is induced by a hormone ………….. .
Answer:
LH
Question 19.
Zygote divides to form ………… which is implanted in uterus.
Answer:
blastocyst
Express the following in one or two word(s)
Question 1.
Give the name of structures by which testes are suspended in the scrotum.
Answer:
Spermatic cords
![]()
Question 2.
Name the cells that nourish the germ cells in the testes. Where are these cells located in the testes?
Answer:
Sertoli cells. They are found on the inner lining of seminiferous tubule.
Question 3.
Name the type of cells found in the secondary follicle.
Answer:
Cuboidal-shaped granulosa cells.
Question 4.
Name the structure formed after the degeneration of corpus luteum.
Answer:
Corpus albicans.
Question 5.
Which hormone is secreted by Leydig cells?
Answer:
Testosterone
Question 6.
Somatic chromosome number is 40.
What shall be the chromosome number in the cells of seminiferous tubules?
Answer:
40 chromosomes
Question 7.
From which part of spermatid is acrosome formed?
Answer:
Head
Question 8.
How many spermatids are produced from a single primary spermatocyte?
Answer:
4
Question 9.
State the stage at which oogonia reach their maximum number.
Answer:
Before birth at five months of foetal life.
Question 10.
When are polar bodies formed in female ovary?
Answer:
During the production of secondary oocyte and ovum.
Question 11.
How many sperms will be produced from 10 primary spermatocytes?
Answer:
40
Question 12.
Name the process of release of spermatozoa from Sertoli cells into cavity of seminiferous tubule.
Answer
Spermiation
Question 13.
Generally, what is the site of.fertilisation in human being?
(Vagina, Uterus, Fallopian tube and Ovary)
Answer:
Fallopian tube
![]()
Question 14.
During fertilisation through which path the male pronucleus moves to meet the female pronucleus?
(Penetration path, Copulation path, Migration path and Zygotic path)
Answer:
Migration path
Question 15.
In which stage of development are the three germinal layers formed ?
Answer:
Gastrula
Question 16.
Which germ layer forms the nervous system?
Answer:
Ectoderm
Question 17.
From which germ layer does the coelom arise in vertebrates?
Answer:
Mesoderm
Question 18.
When does ovulation occur?
Answer:
Day 14 of menstrual cycle
Question 19.
What do you call the layer of cells forming the outer wall of the blastocyst?
Answer:
Trophoblast
Question 20.
Name the thin clear coat surrounding mammalian egg.
Answer:
Plasma membrane
![]()
Short Answer Type Questions
Question 1.
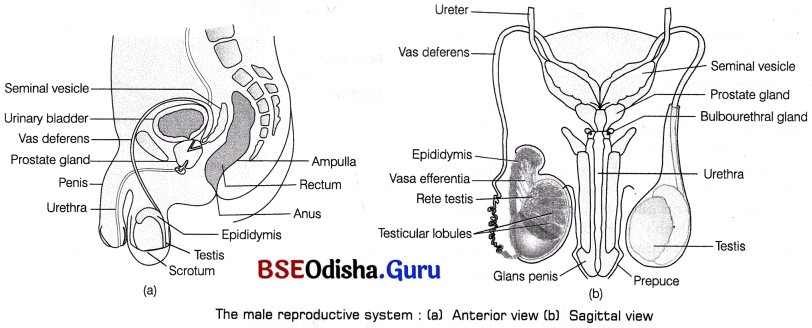
Write a note on human male reproductive system.
Answer:
Human Male reproductive system It consists of various glands, ducts and supporting structures. The structures present in this system are either paired or unpaired.
Testes are primary sex organs, posterior to the penis within the scrotum, produce spermatozoa and testosterone.
Seminal vesicles are club-shaped glands posterior to prostate, secrete alkaline fluid containing nutrients, fructose and prostaglandins.Scrotum is the pouch of skin, posterior to the penis, encloses and protects testes.
Penis is the unpaired organ, anterior to the scrotum and attached to pubis, conveys urine to outside of body.
Prostate gland and Cowper s gland secrete fluids which neutralise acidic environment of vagina and lubricate urethra and penis, respectively.
Question 2.
Draw a labelled diagram of male reproductive system.
Answer:
Question 3.
Why are the human testes located outside the abdominal cavity? Name the pouch in which they are present.
Or
Why are testes extra-abdominal in human males?
Answer:
Human testes are responsible for the synthesis of male gametes (sperms) and they need slightly lower temperature than the normal body temperature for this function. Thus, testes are located outside the abdominal cavity in sac-like structure called scrotum. Its temperature is about 2-3° lower than the normal body temperature.
Question 4.
Describe the structure of a seminiferous tubule.
Or Write a note on seminiferous tubules.
Answer:
Each testicular lobule contains 1-3 highly coiled seminiferous tubules. Each tubule is lined on its inside by two types of cells.
The cuboidal cells are called male germ (spermatogenic) cells and few large pyramidal (supporting cells-Sertoli or Nurse cells).
The former gets divided to form sperms while the latter provides nutrition to the germ cells.
Question 5.
Write the location and function of the following in human testes
(i) Sertoli cells
(ii) Leydig cells
Answer:
(i) Sertoli cells are found in the seminiferous tubules and they help to support and nourish the male gametes.
(ii) Leydig cells are found at interstitial region between seminiferous tubules and secrete androgens.
![]()
Question 6.
What is the significance of epididymis in male fertility?
Answer:
The epididymis helps sperm in attaining maturity, acquiring increased motility and fertilising capacity. It also stores sperms for a short period before they enter the vasa deferens.
Question 7.
How the spermatozoa are moved through the vasa efferentia and the epididymis?
Answer:
Spermatozoa or sperm formed in the seminiferous tubules reaches the vasa efferentia through rete testis. Several vasa efferentia open into the epididymis and carry sperm outside the body.
Question 8.
What are the major components of the seminal plasma?
Answer:
Seminal fluid is a cumulative secretion of accessory sex glands of male that is seminal vesicles, prostate gland and Cowper’s glands. It is rich in fructose, calcium and certain enzymes.
Question 9.
What are the major functions of male accessory ducts and glands?
Answer:
The male accessory ducts are rete testis, vasa efferentia, epididymis and vas deferens. These ducts store and transport the sperms from the testes to the outside through the urethra. The male accessory glands are paired seminal vesicles, prostate gland and paired bulbourethral glands.
The secretion of these glands form seminal plasma, which is rich in fructose, calcium and certain enzymes. The secretion of bulbourethral glands lubricate the penis.
Question 10.
How would a test confirm sexual intercourse by analysing vaginal swab?
Answer:
In this test, vagina is analysed for the presence of fructose, which is not produced anywhere in the human body . except semen (contributed by seminal vesicles). Therefore, its presence in the vagina indicates coitus/sexual intercourse.
Question 11.
Enlist the disorders of male reproductive system.
Answer:
| Disorder | Description |
| Cryptorchidism | Failure of lestes to descend into the scrotum. |
| Benign prostatic hypertrophy | Enlargement of the prostate, often occurs in old age. Causes difficulty in urinating, dribbling and nocturia. |
| Htydrocoele | Accumulation of fluids around a testicle. |
| Erectile dysfunction (impotance) | Inability to develop or maintain an erection of the penis during sexual activity. Causes are drugs, ageing, diabetes, etc. |
| Inguinal hernia | Protrusion of the abdominal cavity contents through the inguinal canal. |
Question 12.
Draw a labelled diagram of female reproductive system.
Answer:
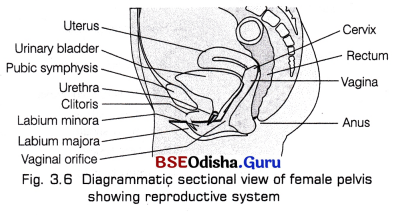
![]()
Question 13.
Write a note on human ovary.
Answer:
Ovaries
Ovaries are the primary sex organs of female that is situated in the pelvic cavity.
They produce female gametes (ovum) and several steroid hormones (ovarian hormones). The ovaries are almond-shaped, lying in the lower part of the abdomen and held to the broad ligament by double folds of peritoneum called mesovarium. Each ovary is about 2-4 cm in length and is connected by an ovarian ligament to the uterus and by a suspensory ligament to the lateral pelvic wall. Each ovary is covered by a thin epithelium layer called germinal epithelium.
Question 14.
What is the difference between a primary oocyte and a secondary oocyte?
Answer:
Primary oocyte is a diploid cell formed in foetal ovary when the gamete mother cell, oogonia is arrested at prophase-I of meiosis. Secondary oocyte is the haploid cell formed from primary oocyte that completes its first meiotic division, during puberty and produces the female gamete ova (n).
Question 15.
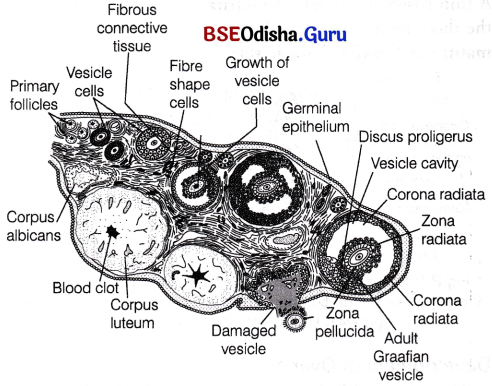
What are the changes in the oogonia during the transition of a primary follicle to Graafian follicle?
Answer:
- The germinal epithelial cells divide repeatedly until many diploid oogonia are formed.
- The oogonia grow to form primary oocytes. Each primary oocyte then gets surrounded by a layer of granulosa cells and is called the primary follicle.
- These get surrounded by more layers of granulosa cells and called secondary follicles.
- The latter soon transforms into a tertiary follicle, which is characterised by a fluid-filled cavity called antrum.
- The primary oocyte within the tertiary follicle undergoes meiotic division to become a secondary oocyte and a first polar body (haploid).
- The tertiary follicle further changes into the mature follicle or Graafian follicle that ruptures to release the secondary oocyte (ovum) from the ovary by the process called ovulation.
Question 16.
Name and explain the role of the inner and middle walls of the human uterus.
Answer:
Uteus has a thick, highly vascular wall composed of three layers of tissues
- Outer perimetrium A thin single-layered membranous covering of uterus wall that is composed of squamous epitbelial cells.
- Middle myometrium A thick layer of smooth muscle fibres, which contracts strongly during the delivery of the baby.
- Inner endometrium A glandular layer with many blood vessels. It consists of simple cuboidal or columnar epithelium. It undergoes cyclic changes during the menstrual cycle.
Question 17.
The diagram shows the side view of the female reproductive system
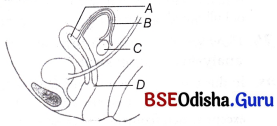
(i) Label the parts A to D.
(ii) In which region are sperms released during intercourse?
Answer:
(i) A-Uterus, B-Fallopian tube, C-Ovary, D-Vagina.
(ii) During intercourse, the penis reaches into the vaginal area and thus, the sperms are released in vagina.
Question 18.
What is spermatogenesis? Briefly describe the process of spermatogenesis.
Answer:
It is the formation of spermatozoa (sperms) in the testes, which originate from the cuboidal cells called Primordial Germ Cells (PGCs). The process of spermatogenesis starts at puberty.
It is completed in two steps
- Formation of spermatids (spermatocytogenesis)
- Transformation of spermatids to sperms (spermiogenesis)
Question 19.
Define spermiogenesis and spermiation.
Or Write a note on spermiogenesis.
Answer:
Spermiogenesis:
It is the formation of spermatozoa (sperms) in the testes, which originate from the cuboidal cells called Primordial Germ Cells (PGCs). The process of spermatogenesis starts at puberty.
It is completed in two steps
- Formation of spermatids (spermatocytogenesis)
- Transformation of spermatids to sperms (spermiogenesis)
Spermiogenesis:
The spermatids (immotile) transform into motile spermatozoa by the process called spermiogenesis. It is also called differentiation phase during which sperm heads get embedded in the Sertoli cells and are finally released from the seminiferous tubules by the process of spermiation.
Question 19.
Draw and label the various parts of human sperm.
Answer:
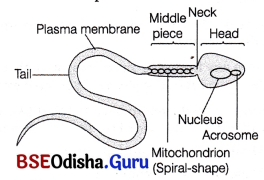
![]()
Question 20.
Spermatogenesis in human males is a hormone regulated process. Justify.
Answer:
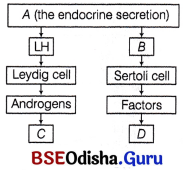
Spermatogenesis initiates due to a significant increase in the secretion of Gonadotropin Releasing Hormone (GnRH) by the hypothalamus at the age of puberty. The increased level of GnRH acts on the anterior pituitary and stimulates the secretion of two gonadotropins, i.e. Luteinizing Hormone (LH) and Follicle Stimulating Hormone (FSH). LH acts on the Leydig cells thus, stimulating the synthesis and secretion of androgens. This in turn stimulate the process of spermatogenesis. FSH acts on Sertoli cells and stimulates the secretion of some factors like inhibins, activins and transferrins which help in spermiogenesis.
Note Androgens are testicular hormones which function to maintain the accessory ducts and glands in males.
Question 21.
State the function of the following
(i) Acrosome
(ii) Sperm tail
Answer:
Their functions are
(i) Acrosome It contains hydrolytic enzymes that are required to dissolve the membranes of the ovum for fertilisation.
(ii) Sperm tail It helps in the sperm movement in the female genital tract for fertilisation.
Question 22.
What is the number of chromosomes in the following cells of a human male?
(i) Spermatogonial cells
(ii) Spermatids
(iii) Primary spermatocytes
(iv) Sertoli cells
Answer:
(i) 46
(ii) 23
(iii) 46
(iv) 46
Question 23.
Identify A, B, C and D with reference to gametogenesis in humans in the flow chart given below.
Answer:
A – GnRH,
B – FSH,
C – Spermatogenesis,
D – Spermiogenesis
Question 24.
Write the steps in the formation of an ovum from an oogonium in human.
Answer:
This process involves following phases
(i) Multiplication phase Cells of germinal epithelium undergo mitotic division to produce undifferentiated germ cells called oogonia or egg mother cells within each foetal ovary.
- The oogonia further divides by mitosis and projects as a chord into the stroma of the ovary. This chord is known as egg tube or pfluger, which later become a round mass called egg nest.
- In the egg nest, one cell grows, enters into prophase-I of meiosis and gets arrested at diplotene stage temporarily. This cell becomes the primary oocyte.
- Other oogonia in the nest surround this primary ooctye to form primary follicle. These follicles protects and nourish the primary oocyte.
- About 2 million of primary follicles exist in females before birth. A large number of these follicles degenerate during the phase from birth to puberty by the process called follicular atresia. Therefore, at puberty only 60000- 80000 primary follicles are left in each ovary.
(ii) Growth phase
- The primary follicles get surrounded by more layers of granulosa cells and a new theca to form secondary follicles.
- This follicle then gets converted into a tertiary follicle that possesses a fluid-filled cavity called antrum surrounded by theca interna and theca externa.
(iii) Maturation phase The primary oocyte within this tertiary follicle grows in size. The fully grown primary oocyte completes its first meiotic division producing two daughter nuclei in which larger haploid cell is called secondary oocyte and the tiny one is called first polar body or polocyte. The secondary oocyte contains bulk of the nutrient rich cytoplasm of primary oocyte and becomes tertiary follicle.
![]()
Question 25.
Why are polar bodies formed during oogenesis, but not in spermatogenesis?
Answer:
Polar bodies are formed during maturation phase of oogenesis. Two small polar bodies are formed during I and II meiotic divisions. Due to unequal cytokinesis, the cytoplasmic content of polar bodies is negligible as compared to ovum. They help to get rid of haploid set of chromosomes during oogenesis. But, during spermatogenesis equal cytokinesis occurs thus, polar bodies are not formed in this.
Question 26.
How many eggs do you think were released by the ovary of a female dog, which gave birth to six puppies?
Answer:
The ovaries of a female dog must have released 6 eggs, each of which was fertilised.
So, six zygotes were formed, that developed into six puppies.
Question 27.
Identify the statements as True/False. Correct each false statement to make it true.
(i) Oogenesis takes place in corpus luteum.
(ii) Spermatozoa get nutrition from Sertoli cells.
Answer:
(i) False-Oogenesis takes place in ovaries.
(ii) True.
Question 28.
What is menstrual cycle? Which hormones regulate menstrual cycle?
Answer:
The hormones that regulate menstrual cycle along with their functions are
- Pituitary gonadotropins (LH, FSH and Oestrogen) These help in the proliferation of Graafian follicle and endometrium of uterus.
- FSH Stimulates the growth of ovarian follicle and secretion of oestrogen.
- Oestrogen Increased level of oestrogen gives positive feedback and stimulates more LH production.
- LH Stimulates ovulation.
- Progesterone Essential for the maintenance of endometrium.
The hormones involved in the process are
- FSH, LH stimulate growth of follicle and maturation of ovum.
- Oestrogen is involved in endometrial repair and growth.
- Oestrogen and progesterone together prepare endometrium and other parts of the body for pregnancy.
Question 29.
Write the source and effect of the high concentration of LH on a mature Graafian follicle.
Answer:
The changes in the ovary during follicular phase stimulates anterior pituitary to release more LH. In the middle of cycle, i.e. during ovulatory phase, LH attains a peak level and it is known as LH surge. High level of LH ruptures the Graafian follicles and thereby releases the ovum.
Question 30.
Draw a labelled diagram of a Graafian follicle.
Answer:
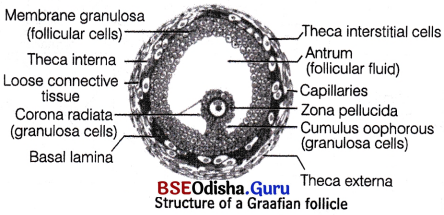
![]()
Question 31.
Describe, how the changing levels of FSH, LH and progesterone during menstrual cycle induce changes in the ovary and the uterus in human female.
Answer:
Both LH and FSH attain a peak level in the middle of cycle (about 14th day).
- Rapid secretion of LH leading to its maximum level during the midcycle is called LH surge. It induces rupture of Graafian follicle and thereby, the release of ovum, i.e. ovulation.
- The ovulation (ovulatory phase) is followed by the luteal phase.
Question 32.
Given alongside is a flowchart showing ovarian change during menstrual cycle. Fill in the spaces with the hormonal factor(s) responsible for the events shown.
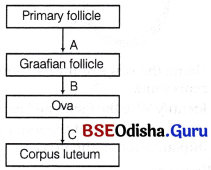
Answer:
A – FSH and oestrogen, B – LH and C – Progesterone.
Question 33.
Corpus luteum in pregnancy has a long life. However, if fertilisation does not take place, it remains active only for 10-12 days. Why?
Answer:
During pregnancy, there is no menstruation. The corpus luteum secretes large amount of progesterone in case the fertilisation occurs.
This is to maintain the corpus luteum as long as the embryo remains there. In the absence of fertilisation, the corpus luteum cannot be maintained for more than 10-12 days and hence, it degenerates.
Question 34.
Write the function of following
(i) Corpus luteum
(ii) Endometrium
Answer:
(i) Corpus luteum It secretes progesterone required for the maintenance of endometrium.
(ii) Endometrium It is the innermost layer of uterus.
It provides nutrition for the development of foetus. Implantation of blastocyst occurs in endometrium.
Question 35.
Write short note on fertilisation.
Or What is fertilisation? In man, where does it take place?
Answer:
Fertilisation:
The process of fusion of a sperm with an ovum is called fertilisation. It involves discharge of semen by the penis into the female’s vagina close to the cervix during coitus is called insemination.
The motile sperms move through the cervix, enter the uterus and reach the junction of the isthmus and ampulla (ampullary-isthmus junction) of the Fallopian tube.
The ovum released from the ovary also reaches the ampullary-isthmic junction, where the two gametic nuclei fuse. This process is called amphimixis or syngamy. Fertilisation can only occur if the ovum and sperms are transported simultaneously to this junction. This explains why all copulations do not lead to fertilisation and pregnancy.
Question 36.
In our society the women are often blamed for giving birth to daughters. Can you explain why this is not correct?
Answer:
Women are blamed for giving birth to daughters. This is wrong because sex of the baby is determined by the sperm that can have either X or Y-chromosomes.
Women have only one type of chromosome (X) in all the ova.
If the sperm having X-chromosome fertilises the ovum (X), the resulting zygote (XX) will become a female.
If the sperm having Y-chromosome fertilises the ovum (X), the resulting zygote (XY) will become a male.
Question 37.
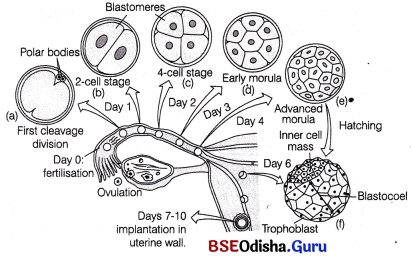
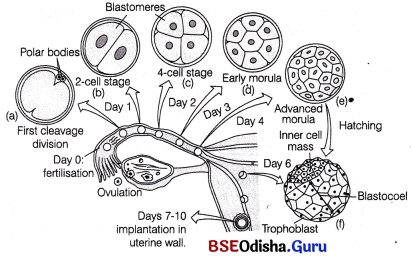
A sperm has just fertilised a human egg in the Fallopian tube. Trace the events that the fertilised egg will undergo upto the implantation of the blastocyst in the uterus.
Answer:
Fertilisation
The process of fusion of a sperm with an ovum is called fertilisation. It involves discharge of semen by the penis into the female’s vagina close to the cervix during coitus is called insemination.
The motile sperms move through the cervix, enter the uterus and reach the junction of the isthmus and ampulla (ampullary-isthmus junction) of the Fallopian tube.
The ovum released from the ovary also reaches the ampullary-isthmic junction, where the two gametic nuclei
fuse. This process is called amphimixis or syngamy. Fertilisation can only occur if the ovum and sperms are transported simultaneously to this junction. This explains why all copulations do not lead to fertilisation and pregnancy.
In humans, fertilisation occurs in following steps
(i) The sperm comes in contact with ovum. The sperm secrete a chemical called anti-fertilizin which react with the chemical called fertilizin secreted by the ovum. This reaction is called agglutination reaction. The fertilizin and anti-fertilizin are complementary only when they belong to same species. This reaction helps to prevent the progress of multiple sperms towards the egg.
(ii) The sperm undergoes capacitadon and acrosomal reacdon. The latter reaction involves the release of sperm lysins which include-hyaluronidase, Corona Penetrating Enzyme (CPE) and Zonalysins (acrosin). These enzymes help in the digestion of primary, secondary egg membranes so that the sperm can penetrate the egg.
(iii) While penetrating the egg, contact between sperm and zona pellucida depolarise the membrane (fast block) so as to block the entry of additional sperms. Similarly, the contact between sperm and corona radiata induces cortical reaction (slow block and results in the formation of a fertilisation membrane.
(iv) Simultaneously, secondary oocyte restart cell cycle by the breakdown of MPF to APC (Anaphase Promoting Complex) due to the entry of sperm.
(v) After the completion of second meiotic division, ovum is formed. Its nucleus condenses to form female pronucleus. Simultaneously, male pronucleus is formed by the separation of sperm head from middle piece.
(vi) The fusion of male and female pronuclei results in the formation of zygote (2n – 46).
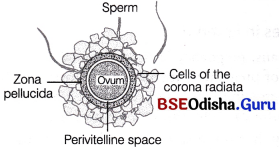
Ovum surrounded by sperms
![]()
Question 38.
Name the embryonic stage that gets implanted in the uterine wall of the human female. Also draw its diagram.
Answer:
The blastocyst gets embedded in the endometrium of the uterus.
This is called implantation and it leads to pregnancy.
Question 39.
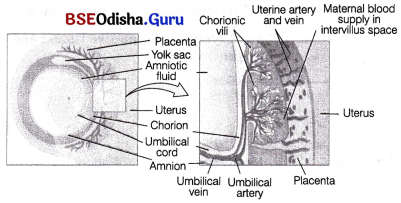
When and where do chorionic villi appear in humans? State their function.
Answer:
Chorionic villi appear just after implantation. They appear as finger-like projections on the trophoblast and become interdigitated with the surrounding uterine tissues and form the placenta.
Question 40.
A woman passes out hCG in the urine during the pregnancy. Why?
Answer:
The presence of human Chorionic Gonadotropin (hCG) is the basis of pregnancy test. Placenta formed during pregnancy releases hCG, which comes in urine of pregnant woman.
Question 41.
Mention the name of hormones and their source organs produced only during pregnancy.
Answer:
The hormones are
(i) human Chorionic Gonadotropin (hCG) It is secreted by the placenta.
(ii) Relaxin It is secreted by the ovary.
Question 42.
Placenta acts as an endocrine gland. Explain.
Or
Write the function of placenta.
Or
Write a note on placenta.
Answer:
The placenta secretes hormones like human gonadotropins, human placental lactogen, oestrogen and progesterone that are necessary to maintain pregnancy. Due to the secretion of these hormones, it is called an endocrine gland.
Question 43.
When and how does placenta develop in human female?
Answer:
Soon after implantation, finger-like projections appear on k the trophoblast. These are known as chorionic villi and surrounded by the uterine tissue and maternal blood.
The chorionic villi and the uterine tissue become inter-digitated with each other. Together, they form a structural and functional unit between foetus and maternal body called placenta. In humans the placenta is of haemochorial metadiscoidal and deciduous type. After the sixth week of pregnancy, placenta take over the function of corpus luteum and produce oestrogen and progesterone.
Question 44.
Where is morula formed in humans? Explain the process of its development from zygote.
Answer:
The development of embryo from fertilised ovum involves the following events. The mitotic division starts as the zygote (fertilised ovum) moves through the isthmus of the oviduct towards the uterus, forming 2, 4, 8, 16 daughter cells called blastomeres. This process is called cleavage. During holoblastic cleavage in humans, the young embryo is slowly moving down the Fallopian tube towards the uterus and following events take place
- The embryo with 8-16 blastomeres is called morula, But, it is not larger than a zygote.
- The morula continues to divide and transforms into blastocyst as it moves further into the uterus. The cavity of the blastocyst is called blastocoel. This process of transformation is called blastulation.
- The blastomeres in the blastocyst are arranged into an outer layer called trophoblast and the inner group of cells attached to trophoblast called the inner cell mass.
- The trophoblast layer then gets attached to the endometrium and the inner cell mass differentiates into the embryo. After attachment, the uterine cells divide rapidly and cover the blastocyst.
- As a result, the blastocyst becomes embedded in the endometrium of the uterus. This is called implantation and it leads to pregnancy (i.e. the time from conception to birth).
![]()
Question 45.
State the function of yolk.
Answer:
The function of yolk are
- It provides nutrition to the developing embryo.
- Cleavage, i.e. the division of cells in the early embryo mostly depends on the amount of yolk in the egg.
- The cleavage can be holoblastic (total cleavage) or meroblastic (partial cleavage).
Question 46.
What is the effect of yolk on cleavage?
Answer:
- The zyogte undergoes mitotic divisions called cleavage and develops into an embryo.
- The pattern of cleavage is determined by the amount of yolk and its distribution in the egg.
- If the egg is having moderate to sparse amounts of yolk then the egg divides completely and this type of cleavage is called holoblastic cleavage.
- If the egg contains a large amount of yolk then the egg cannot divide completely as the cleavage furrow cannot penetrate the yolk. This type of cleavage is called meroblastic cleavage.
Question 47.
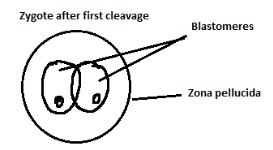
Draw the following diagrams related to human reproduction and label them.
(i) The zygote after first cleavage division
(ii) Morula stage
(iii) Blastocyst stage (sectional view)
Answer:
(i) The zygote after first cleavage division
(ii) Morula stage
(iii) Blastocyst stage (sectional view)
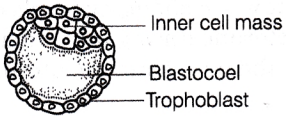
Question 48.
Study the figure given below and answer the questions that follows.
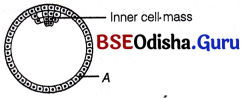
(i) Name the stage of human embryo the figure represents.
(ii) Identify ‘A’ in the figure and mention its function,
(iii) Mention the fate of the inner cell mass after implantation in the uterus.
Answer:
(i) Blastocyst.
(ii) ‘A’ is trophoblast. The trophoblast layer gets attached to endometrium and later forms chorionic villi.
(iii) The inner cell mass gets differentiated into an embryo.
Question 49.
What is parturition? Which hormones are involved in induction of parturition?
Or
Why parturition is called a neuroendocrine mechanism? Explain.
Or
What are gestation and parturition?
Answer:
Parturition
The time period during which the embryo remains in the uterus, i.e. after the last day of menstruation to the day of parturition is called gestation. The gestation period of humans is about 9 months.
Vigorous contraction of the uterus at the end of pregnancy causes expulsion/delivery of the foetus. This process of delivery of the foetus (childbirth) is called parturition. It is induced by a complex neuroendocrine mechanism.
The signals of parturition originate from the fully developed foetus and the placenta, which induce mild uterine contractions. It is called foetal-ejection reflex.
- This triggers the release of oxytocin from the maternal pituitary. It promotes contractions of uterine muscles, which in turn stimulate further secretion of oxytocin.
- The stimulatory reflex between the uterine contraction and oxytocin secretion continues resulting in stronger contractions. This leads to the expulsion of the baby out of the uterus through the birth canal.
- Soon after the birth of baby, placenta is also expelled out of the uterus. Relaxin hormone relaxes the pelvic ligaments of mother to prepare for the childbirth.
Question 50.
What is lactation? Mention its significance.
Answer:
Lactation:
The mammary glands in females undergo differentiation during pregnancy. The production and release of milk by the mammary glands of female after birth of a young one is called lactation. The first milk, which comes out from the mother’s mammary glands just after childbirth is called colostrum. It is rich in proteins and energy along with the Antibodies (IgA) that provide passive ‘ immunity to the newborn. Breast feeding during the initial period of infant growth is highly recommended by the doctors for bringing up a healthy baby.
![]()
Differentiate between the following (for complete chapter)
Question 1.
Graafian follicle and Corpus luteum.
Answer:
Differences between Graafian follicle and corpus luteum are as follows
| Graafian follicle | Corpus luteum |
| It consists of an oocyte, zona pellucida, cellular membranous granulosa surrounded by the theca interna and the externa. | It consists of luteum cells, fibrin and blood clot. |
| It contains follicular antrum (follicular cavity) filled with follicular fluid. | It contains blood clot. |
| It is formed by the germinal epithelium of the ovary. | It is formed after the release of secondary oocyte from the Graafian follicle. |
| Its granular cells secrete oestrogens. | It secretes progesterone. |
Question 2.
Corpus luteum and Corpus albicans.
Answer:
Differences between corpus luteum and corpus albicans are as follows
| Corpus luteum | Corpus albicans |
| Graafian follicle changes into corpus luteum after ovulation in ovary. | Corpus luteum degenerates and forms corpus albicans if there is no pregnancy. |
| It is made of luteal cells. | It is made of scar tissues. |
| Secretes progesterone. | Do not secrete any hormone. |
Question 3.
Menarche and Menopause.
Answer:
Differences between menarche and menopause are as follows
| Menarche | Menopause |
| It is the first menstrual period in human female. | It is the end of menstrual period in human female. |
| It occurs at around 11-16 years of age. | It occurs at around 45-50 years of age. |
| It marks the beginning of reproductive phase of a female. | It marks the end of reproductive phase of a female |
| There is elevated level of oestrogen. | There is decline in the level of oestrogen. |
![]()
Question 4.
Endometrium and Myometrium.
Answer:
Differences between endometrium and myometrium are as follows
| Endometrium | Myometrium |
| It is inner glandular layer of the wall of the uterus. | It is thick muscular middle layer of the wall of the uterus. |
| It undergoes cyclic changes during menstrual cycle. Implantation of blastocyst takes place on endometrium. | It is involved in the uterine movements. |
Question 5.
Spermatocytes and Oocytes.
Answer:
Differences between spermatocytes and oocytes are as follows
| Spermatocytes | Oocytes |
| Primary spermatocytes are formed from the spermatogonia in the seminiferous tubules of testes by mitosis. | Primary oocytes are formed from the oogonia in the ovary of the foetus. |
| Each primary spermatocyte undergoes meiosis-i and forms the two haploid secondary spermatocytes. | Each primary oocyte undergoes meiosis-l and forms haploid secondary oocytes and haploid first polar body. |
| Each secondary spermatocyte undergoes meiosis-ll and forms two haploid spermatids. | The secondary oocyte undergoes meiosis-ll and forms one ovum and one second polar body. |
| Each primary spermatocyte forms four haploid spermatids. | Each primary oocyte forms one ovum and three polar bodies. |
Question 6.
Cleavage and Typical mitosis.
Answer:
Differences between cleavage and typical mitosis are as follows
| Cleavage | Typical mitosis |
| It occurs in zygote or parthenogenetic egg, | It occurs in most of body cells. |
| Interphase is short. | Interphase is of long duration. |
| Growth does not occur. | Growth occurs during interphase. |
| Oxygen consumption is high as it is very rapid process. | Oxygen consumption is low as it is slow process. |
| Size of blastomeres decreases. | Size of daughter cells remains same after growth. |
| DNA synthesis is faster. | DNA synthesis is slower. |
| Nuclear cytoplasmic ratio increases. | Nuclear cytoplasmic ratio remains same. |
Long Answer Type Questions
Question 1.
Give an account of the human male reproductive system.
Answer:
Human Reproductive System
Human beings show prominent sexual dimorphism in which male and female differ from each other by a number of primary and secondary sex characters. Primary sex characters are those which are present since birth in both males and females, e.g. external genitalia.
The secondary sex characters appear after puberty and include a number of traits like the presence of thick facial hairs, low pitch voice, etc., in males and well-developed mammary glands, high pitch voice, etc., in females.
On the basis of their functions, reproductive organs can be divided into the following types
- Primary sex organs These produce gametes and sex hormones, e.g. ovary in females and testes in males.
- Secondary sex organs These do not produce gametes or sex hormones, but help in morphological discrimination among two sexes, e.g. breast in females, penis in males, etc.
- Accessory organs These do not form gametes, but are essential for reproduction, e.g. prostate gland in males, Fallopian tube in females,
Male Reproductive System:
The male reproductive system is located in the pelvis region. It consists of scrotum a pair of testes, excurrent ducts and accessory glands.
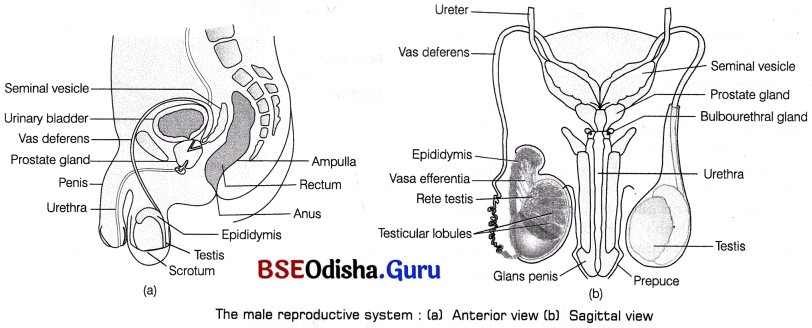
The male reproductive system : (a) Anterior view (b) Sagittal view
Scrotum:
It is a pouch-like structure of pigmented skin arising from the lower abdominal wall and hanging between the leg. It is divided internally into right and left scrotal sacs by a muscular partition called septum scrota. The testis originates in the abdominal cavity, but later during the seventh month of development, it descend into the respective scrotal sacs through the passages called inguinal canals.
Testicular descent to inguinal region during gestation period is affected by Antimullerin Hormone (AMH) secreted by Sertoli cells. 90% of babies have completely descended testes, when they are born. In 10% of new-borns, testes fail to descend and retained in the abdominal cavity. This condition is called cryptochidism. It can be treated by gonadotropins or surgery.
In cold weather, the testes are elevated by the contraction of a band of muscle, known as cremasteric muscle to get the warmth of the trunk. This effect is known as cremasteric reflex.
The same effect occurs when the thigh of a man is stroked. In the baby, this stimulus causes the testes to ascend up into the abdominal cavity through the inguinal canal.
Functions of Scrotum:
Scrotum keeps the temperature of testes about 2-2.5°C lower than the internal body temperature, which is essential for the production of sperms, i.e. spermatogenesis. This temperature is maintained by perspiration and evaporation from the scrotal surface. These processes occur due to the presence of pampiniform plexus that surround testiculae arteries which ascend from the testis. Venous blood returning from testis through pampiniform plexus is cooler than the blood in testicular arteries. The countercurrent heat exchange mechanism between the arterial and venous blood cools down the arterial blood.
Testes: Microscopic Anatomy:
Testes are the primary sex organs in men. These are the male gonads, i.e. the site where the male gametes or sperms are made. A pair of testis is situated outside the abdominal cavity within the scrotum. Each testis is oval in shape and measures about 4-5 cm in length and 2-3 cm in width. These are suspended in the scrotum by spermatic cords.
Microscopic Anatomy:
The outermost covering of the testis is formed by a dense connective tissue called tunica albuginea. It thickens and extends inwardly into each testis as mediastinum testis which further forms thin connective tissue septum. The latter divides each testis into 200-300 compartments called testicular lobules. Each lobule contains 1-3 highly convoluted seminiferous tubules that is lined by stratified cuboidal epithelium.
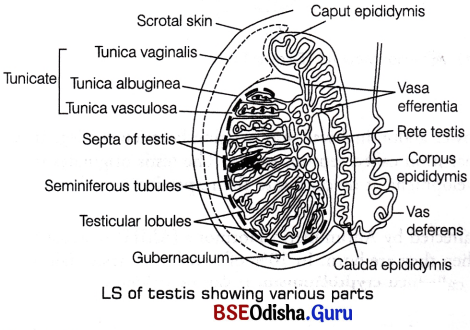
Seminiferous Tubule:
It is the structural and functional unit of testis in which sperms are produced. Each seminiferous tubule is present in the mass of loose connective tissue that contain fibroblast, epithelial cells, nerves, blood and lymphatic vessels, etc. Inside these tubules, two types of highly specialised cells are present namely Sertoli cells (nurse cells) and spermatogenic cells.
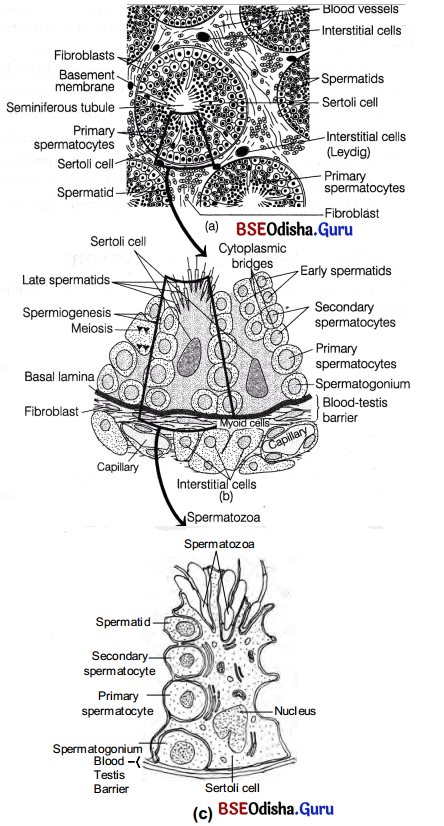
Transverse section through human testis : (a) A single seminiferous tubule with cells of Leydig in the interstitial tissue, (b) A magnified part of the seminiferous tubule showing the blood-testis barrier, Sertoli cells and its relationship to the differentiating spermatogenic cells and (c) A Sertoli cell with spermatogenic cells in different stages of development
1. Spermatogenic cells These are majority of dividing cells or male germ cells (cuboidal cells) which produce spermatogonia by mitotic division. The spermatogonia further grows into primary spermatocytes and undergo meiosis producing haploid cells, first secondary spermatocytes and then spermatids.
2. Sertoli or Sustentacular cells They are tall, pyramidal, non-dividing somatic cells. They serve the supporting and nourishing function for the spermatogenic cells in different stages of their differentiation. The basal lamina of the germinal epithelium, muscle-like myoid cells at the base of the basal lamina and tight junctions between adjacent Sertoli cells constitute a blood testis barrier which performs the following functions
Prevents many macromolecules from moving into the tubular lumen.
Prevents the blood borne noxious chemical agents from entering into the tubule.
Prevents the passage of antigenic agents from the tubule into the blood, which are likely to generate an autoimmune response.
The region outside the seminiferous tubules called interstitial spaces contain small blood vessels and masses of cells called interstitial cells or Leydig cells. These cells synthesise and secrete the testicular hormones called androgens. Leydig cells are endocrine in function and thus, regulate and maintain male sex characteristics. Other immunologically competent cells are also present in this region.
Accessory or Excurrent Duct System:
These ducts store and transport the sperms along with other glandular secretions from the testis to the outside through urethra. The male’s sex accessory ducts include-tubuli recti, rete testis, vasa efferentia (intratesticular ducts), epididymis, vas deferens and urethra (extratesticular ducts). The ends of seminiferous tubules converge and join to form short straight tubules called tubuli recti.
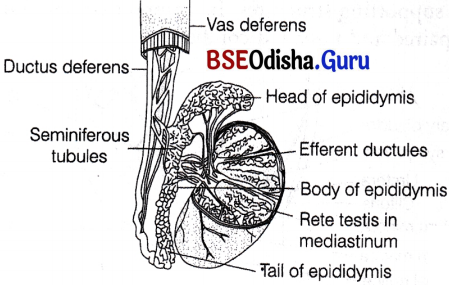
Duct system in human testis
The tubuli recti open into a network of wider, irregular tubules called rete testis, that further open into 12 short efferent ductules or ductuli efferentes.
The latter open into the epididymis and carry sperms outside the testis. Epididymis is a long tube, which is greatly coiled and tightly packed to form an elongated flattened body. It is located along the posterior surface of each testis.
Sperms undergo physiological maturation, acquiring increased motility and fertilising capacity (i.e. capacitation) in epididymis. After that, they pass down to the tail of epididymis, where they stay for a very short period before entering the two vas deferens or ductus deferens.
The vas deferens ascends to the abdomen and lopps over urinary bladder. It receives a duct from seminal vesicle to form ejaculatory duct. The ejaculatory duct enters the prostate gland and opens into the prostatic urethra.
The prostatic urethra extends through the penis to its external opening called urethral meatus or penile urethra. The urethra carries urine from bladder as well . as spermatozoa and secretions from the Cowper’s and prostate glands.
Accessory Glands:
The accessory glands or the secondary glands in males are described below
1. Prostate gland It is a single gland that lies inferior to the bladder. It receives two ejaculatory ducts that joins to form prostatic urethra. The latter receives ductules from prostate. It secretes a milky, slightly alkaline fluid, that contains lipids, enzymes, citric acid, etc.
It is released during ejaculation and helps to neutralise the acidic medium of vagina, making sperms more active to swim. Prostatic fluid accounts for nearly 20-30% of semen volume.
2. Seminal vesicles This paired gland is present posterior to the bladder above prostate. Its ducts empties in the ampulla of ductus deferens.
They secrete mucus and a watery alkaline fluid that contains fructose (acts as an energy source for the sperms). Prostaglandins (stimulate uterine contractions for sperm movement) and a clotting protein form a temporary clot after ejaculation. Later, fibrolysins dissolves the coagulate or clot so that it assume a liquid form. Calcium and certain other enzymes are also a part of seminal plasma.
Fructose, produced by seminal vesicles, is not present elsewhere in the body. Therefore, during forensic test for rape, its presence in females genital tract confirms sexual intercourse. The seminal vesicles and prostrate degenerates or atrophy after the removal of testes because they are androgen dependent glands.
3. Bulbourethral or Cowper’s gland These are situated beneath the bladder and behind the urethra. There ductules discharge into the prostatic urethra. They secrete mucus and an alkaline fluid into the urethra. The mucus helps in the lubrication of penis and neutralises any urinary acids in urethra
Semen
The secretions of accessory sex glands (seminal plasma) and mucus are added to the sperms to form seminal fluid or semen. The main constituent of the semen is live spermatozoa present in an alkaline viscous medium. It is maintained at a pH range of 7.2-7.8. Another main constituent is fructose contributed by the seminal vesicles. It is the chief energy source for the spermatozoa.
The semen is forcibly expelled through the urethra by the process known as ejaculation. The volume of ejaculate is 1.5-5.0 mL. The normal count of sperm is 40-250 million/mL. The secretions have many functions
- Provide medium for transport of sperms.
- Nourish and activate sperms to keep them viable and motile.
![]()
Question 2.
Study the given figure.

(i) Pick out and name the cells that undergo spermiogenesis.
(ii) Name ‘A’ and ‘B ’ cells. What is the difference between them with reference to the number of chromosome?
(iii) Pick out and name the motile cells.
(iv) What is ‘F’ cell? Mention its function.
(v) Name the structure of which the given diagram is a part.
Answer:
(i) A-Spermatids, undergo spermiogenesis.
(ii) A-Spermatids, B-Spermatogonium.
Spermatogonium (B) are diploid and have 46-chromosomes in humans while, spermatids (A) are haploid and have 23-chromosomes in case of human male.
(iii) E-Spermatozoa, are motile cells.
(iv) F-Sertoli cell, it provides nutrition to the germ cells.
(v) Seminiferous tubule.
Question 3.
Give an account of the human female reproductive system.
Answer:
Female Reproductive System:
It consists of a pair of ovaries, glands, a duct system and many supporting structures. Its components are found in both paired and unpaired condition.
The female reproductive system consists of the following organs
Ovaries:
Ovaries are the primary sex organs of female that is situated in the pelvic cavity.
They produce female gametes (ovum) and several steroid hormones (ovarian hormones). The ovaries are almond-shaped, lying in the lower part of the abdomen and held to the broad ligament by double folds of peritoneum called mesovarium. Each ovary is about 2-4 cm in length and is connected by an ovarian ligament to the uterus and by a suspensory ligament to the lateral pelvic wall. Each ovary is covered by a thin epithelium layer called germinal epithelium.
Next to this layer, dense irregular connective tissue mass called tunica albuginea is present. Inner to this, cortex is present which is followed by highly vascularised connective tissue called cortex or stroma ovarian stroma, which contains connective tissues, blood vessels and mature follicles. The stroma is divided into two parts, i.e. a peripheral cortex and an inner medulla or stroma. There is no distinct boundary between the cortex and medulla.
Microscopic Anatomy of Ovary:
The production of eggs in females begins before birth, i.e. during the embryonic development stage, but is completed only after fertilisation. It takes place in ovaries. Cells of germinal epithelium undergo mitotic or equational division during multiplication phase, producing undifferentiated germ cells called oogonia or egg mother cells within each foetal ovary.
These cells enter into the phase of maturation and start two meiotic divisions to enter prophase-I of meiotic division as primary oocytes. They get temporarily arrested at diplotene state and remains as such until the onset of puberty.

Primordial and primary follicles in the cortex of the ovary
Each primary oocyte then gets surrounded by a single layer of squamous follicle cells and is called the primordial follicle. About 2 million of these follicles exist in ovarian cortex of females before birth. A large number of these follicles degenerate during the phase from birth to puberty. Therefore, at puberty only 60000-80000 primary follicles are left in each ovary.
The primordial follicles get surrounded by more layers of cuboidal granulosa cells and a new theca. This process is stimulated by the pituitary gonadotropins-FSH and LH. Later the squamous follicular cells of primordial follicle changes to cuboidal or low columnar cells. This follicle is called primary follicle.
The follicular cells of primary follicle divide by mitosis and forms the new cuboidal-shaped granulosa cells. At this stage follicle is called secondary follicle.
The innermost layer of granulosa cells is corona radiata that surrounds the oocyte. Between the oocyte and eorona radiata, a glycoprotein layer called zona pellucida appears. The stromal cells that surround granulosa cells differentiate to form thecal cells. These cells differentiate as an outer theca externa and inner theca interna.
A thin basement membrane separates granulosa cells from the theca interna. This follicular stage is known as mature or Graafian follicle stage.
Structure of a Graafian (mature) follicle : A part(inset) is magnified to show the elaborate structure of the egg with the associated follicle cells
Development of Ovarian Follicle:
- The primary follicle grow in size and a fluid called liquor folliculi or follicular fluid accumulates in a cavity called antrum of granulosa cells. These follicles with an antrum are called antral or secondary follicles.
- The synthesis of liquor folliculi continues, antrum grows in volume and further segregation of granulosa cells occur. Due to this, few cells surround the oocytes and some other are displaced to periphery.
- Theca externa cells form multiple layers around theca interna cells which leads to the formation of mature or Graafian follicle. At this stage, the first meiosis of primary oocyte gets completed to form a secondary oocyte.
- The Graafian follicle, ruptures to release the secondary oocyte from the ovary.
- The secondary ooctye is captured by the fimbriae of Fallopian tube which transport it to the uterus.
- The remaining portion of Graafian follicle gets filled with blood to form corpus haemorrhagicum.
- The theca and granulosa cells proliferate and become glandular to form theca lutein and granulosa lutein cell, respectively. These lutein cells are the source of oestrogen and progesterone. This post ovulatory follicle is called corpus luteum (endocrine structure) which secrete estradiol, progesterone and relaxin (peptide hormone).
Fate of Corpus Luteum:
- If fertilisation occurs Corpus luteum persist and no mensuration occurs, zygote undergoes embryonic development and implants in the endometrium of uterus.
- If fertilisation does not occur Corpus luteum degenerates to form corpus albicans and menstruation occurs.
Not all ovarian follicles reach maturity. Only one dominant follicle gets matured and ovulated. Rest of them degenerates by the process called follicular atresia and the resultant follicles are known as atretic follicles which are replaced by connective tissue.
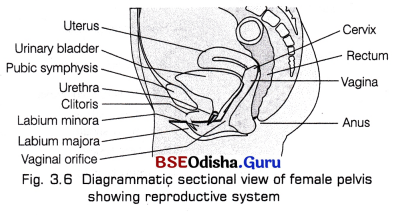
Fallopian Tube (Uterine Ducts):
These are two small accessory tubes of 10-12 cm length, lying on either sides of uterus near the kidney. These tubes carry the egg from the ovary to the uterus and also provides the appropriate environment for its fertilisation.
The Fallopian tubes or oviducts show four regions, i.e. infundibulum, ampulla, isthmus and interstitial region,
- Infundibulum is broad and funnel-shaped with its edges bearing motile, finger-like projections called fimbriae. It helps in the collection of ovum after ovulation.
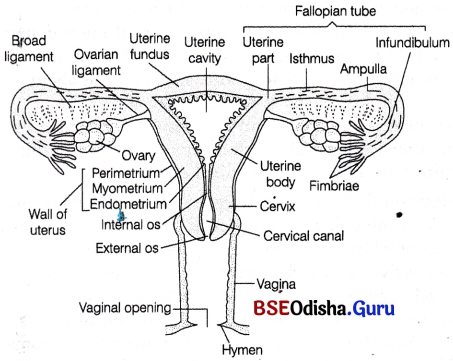
Female reproductive system - Ampulla is the long, wide, thin-walled part of the Fallopian tube next to the infundibulum where fertilisation takes place.
- Isthmus is a short narrow lumen that follows ampulla and joins the uterus.
- Interstitial region passes through the uterine wall and communicates with the uterine cavity.
Uterus (Womb):
It is about 7.5 cm long, 5 cm wide, like an inverted pear in shape. It is supported by ligaments attached to the pelvic wall. It lies between the urinary bladder and rectum.
Uterus has a thick, highly vascular wall, composed of three layers of tissues
- Outer perimetrium A thin single-layered membranous covering of uterus wall that is composed of squamous epithelial cells.
- Middle myometrium A thick layer of smooth muscle fibres, which contracts strongly during the delivery of the baby.
- Inner endometrium A glandular layer with many blood vessels. It consists of simple cuboidal or columnar epithelium. It undergoes cyclic changes during the menstrual cycle.
Blood Supply to Uterus:
The arteries that supply blood to uterus gets divided into arcuate arteries and spreads in the myometrium. The arcuate arteries further gets divided into parts so as to supply blood to endometrium.
These include
- Straight arteries These are short, supply blood to basalis layer.
- Spiral arteries These are long and coiled, supply blood to functionalis layer. Decreased supply to this layer during menstruation causes it to degenerate and cast off.
The endometrium descends into the lamina propria and form numerous uterine glands. Functionally, the layer is divided into two layers
- Luminal stratum functionalis During menstruation, this layer cast off along with blood vessels and uterine glands.
- Stratum basalis It helps to form a new functionalis layer.
Functions of Utreus:
Uterus receives the ovum from the Fallopian tube, forms placenta for the development of foetus and also expels the young one at the time of birth.
Cervix:
It is the narrow entrance of the uterus into the vagina. It has strongest sphincter in its wall and is normally blocked by a plug of mucus. The cavity of cervix is called cervical canal which along with vagina forms the birth canal.
Vagina:
It is about 10 cm long and acts as a receptacle for the penis during copulation, for allowing menstrual flow and for serving as a birth canal during parturition. It opens to the exterior by an aperture called vaginal orifice situated posterior to the opening of urethra.
Accessory Glands:
1. A pair of greater vestibular or Bartholin’s gland occurs on each side of the vaginal orifice. They are small rounded bodies.
These glands correspond-to the Cowper’s gland of the male and secrete a clear, viscid fluid under sexual excitement. This fluid serves as a lubricant during copulation.
2. Numerous glands of skene are present on either sides of urethral orifice. They are homologous to male’s prostate and secrete mucus. These are also called lesser vestibular or paraurethral glands.
External Genitalia (Vulva):
The external genitalia of females consists of the following parts
1. Mons pubis It is the anteriormost structure of vulva and is covered with skin and pubic hairs.
2. Two longitudinal folds of tissue called labia majora form the boundary of the vulva. It also covers two additional folds of tissue called the labia minora.
Both labia majora and labia minora protect the vaginal and urethral openings.
3. Clitoris It is the small erectile organ, which lies at the upper junction of the labia minora above the urethral opening. It is a homologous structure to glans penis of males.
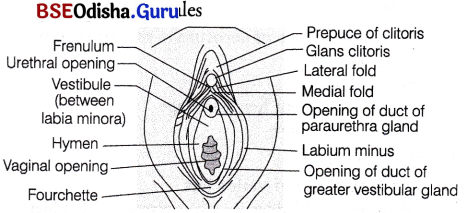
Frontal view of vagina with its associated structures
4. Hymen The vaginal orifice is normally covered by a membrane, called hymen. It is a thin mucous membrane, which covers the vaginal opening either partly or completely. It is often torn during the first coitus (intercourse), but may be present in some women even after coitus. Hymen may also get stretched or torn by normal activities such as horseback riding and therefore, the presence or absence is not an accurate indicator of a woman’s virginity or sexual experience.
![]()
Question 4.
Illustrate in detail the process of spermatogenesis in human.
Or Describe the process of spermatogenesis.
Answer:
Spermatogenesis:
It is the formation of spermatozoa (sperms) in the testes, which originate from the cuboidal cells called Primordial Germ Cells (PGCs). The process of spermatogenesis starts at puberty.
It is completed in two steps
- Formation of spermatids (spermatocytogenesis)
- Transformation of spermatids to sperms (spermiogenesis)
Spermatocytogenesis
It includes the following stages
1. Multiplication phase The undifferentiated germ cells present on the inside wall of seminiferous tubules of the testes are called spermatogonia (sing : spermatogonium) or sperm mother cells. They increase in number by repeated mitotic divisions so that the newly formed spermatogonium possesses the same number of chromosomes.
Each spermatogonium is diploid and contains 46-chromosomes.
2. Growth phase Some of the spermatogonia grow by obtaining nourishment from Sertoli cells and differentiate to primary spermatocytes.
3. Maturation phase or Formation of spermatids Each of these primary spermatocytes undergoes first meiotic division (reductional) and produces two secondary spermatocytes (23-chromosomes) each which further undergoes second meiotic division (equational) to produce four haploid spermatids.
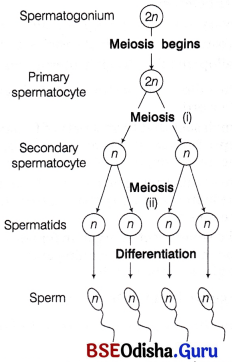
Spermiogenesis:
The spermatids (immotile) transform into motile spermatozoa by the process called spermiogenesis. It is also called differentiation phase during which sperm heads get embedded in the Sertoli cells and are finally released from the seminiferous tubules by the process of spermiation.
Hormones Essential for Spermatogenesis
Spermatogenesis initiates due to a significant increase in the secretion of Gonadotropin Releasing Hormone (GnRH) by the hypothalamus at the age of puberty. The increased level of GnRH acts on the anterior pituitary and stimulates the secretion of two gonadotropins, i.e. Luteinizing Hormone (LH) and Follicle Stimulating Hormone (FSH). LH acts on the Leydig cells thus, stimulating the synthesis and secretion of androgens. This in turn stimulate the process of spermatogenesis. FSH acts on Sertoli cells and stimulates the secretion of some factors like inhibins, activins and transferrins which help in spermiogenesis.
Question 5.
(i) When and where does spermatogenesis occur in a human male?
(ii) Draw the diagram of a mature human male gamete. Label the following parts: acrosome, nucleus, middle piece and tail.
(iii) Mention the functions of acrosome and middle piece.
Answer:
(i) Spermatogenesis occurs at the age of puberty in testes.
(ii)
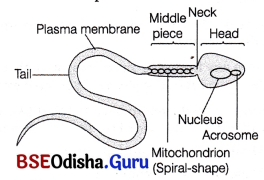
(iii) Head It is flat, oval and composed of a large haploid nucleus and a small anterior cap-like structure, called acrosome. The acrosome lies at the tip of the nucleus and is formed from the Golgi complex. It contains hydrolytic enzymes and is used to contact and penetrate the egg (ovum) during fertilisation.
(ii) Middle piece It is cylindrical and known as the , powerhouse of the sperm. It possesses many mitochondria to produce energy for the movement of the tail that facilitates sperm motility essential for fertilisation.
Question 6.
What is oogenesis? Give a brief account of oogenesis.
Or Write a note on oogenesis.
Or Describe the process of oogenesis.
Answer:
Oogenesis:
It is the process of formation of a mature female gamete called egg or ova. The production of eggs in females begins before birth, i.e. during the embryonic development stage, but is completed only after fertilisation. It takes place in ovaries.
This process involves following phases
(i) Multiplication phase Cells of germinal epithelium undergo mitotic division to produce undifferentiated germ cells called oogonia or egg mother cells within each foetal ovary.
- The oogonia further divides by mitosis and projects as a chord into the stroma of the ovary. This chord is known as egg tube or pfluger, which later become a round mass called egg nest.
- In the egg nest, one cell grows, enters into prophase-I of meiosis and gets arrested at diplotene stage temporarily. This cell becomes the primary oocyte.
- Other oogonia in the nest surround this primary ooctye to form primary follicle. These follicles protects and nourish the primary oocyte.
- About 2 million of primary follicles exist in females before birth. A large number of these follicles degenerate during the phase from birth to puberty by the process called follicular atresia. Therefore, at puberty only 60000- 80000 primary follicles are left in each ovary.
(ii) Growth phase
- The primary follicles get surrounded by more layers of granulosa cells and a new theca to form secondary follicles.
This follicle then gets converted into a tertiary follicle that possesses a fluid-filled cavity called antrum surrounded by theca interna and theca externa.
(iii) Maturation phase The primary oocyte within this tertiary follicle grows in size. The fully grown primary oocyte completes its first meiotic division producing two daughter nuclei in which larger haploid cell is called secondary oocyte and the tiny one is called first polar body or polocyte. The secondary oocyte contains bulk of the nutrient rich cytoplasm of primary oocyte and becomes tertiary follicle.
- Tertiary follicle changes into mature Graafian follicle. Zona pellucida that is formed by secondary oocyte, surrounds it.
- Graafian follicle ruptures to release secondary oocyte. This process is called ovulation.
- The secondary oocyte completes its maturation in Fallopian tube by second maturation division (unequal division), which is triggered by sperm penetration (egg activation) and leads to the formation of ootid and a second polar body. First polar body usually degenerates during this division.
The ootid undergoes few changes and gets transformed into mature ovum or egg, which is ready to be fertilised.
